Celiac Plexus
Introduction
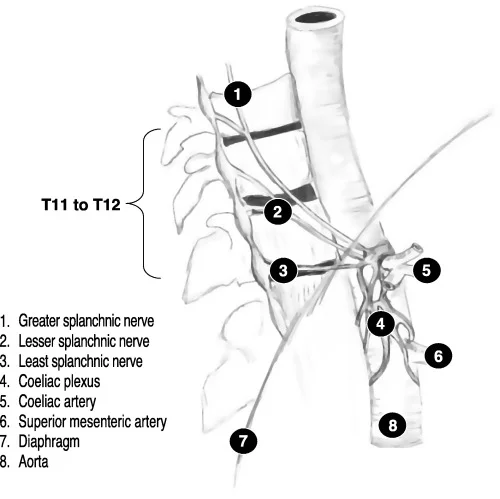
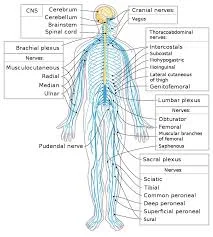
The celiac plexus, also known as the solar plexus, is a network of nerves located in the upper abdomen, near the aorta and behind the pancreas. It plays a key role in transmitting signals between the abdominal organs and the central nervous system.
The celiac plexus is often targeted for nerve blocks to manage chronic abdominal pain, particularly in conditions like pancreatic cancer or chronic pancreatitis.
Receiving parasympathetic and sympathetic inputs from the vagus (CN X) and splanchnic nerves, as well as transmitting their corresponding postsynaptic outputs to the abdominal viscera, is the role of the celiac plexus.
Structure
Several minor plexuses are part of the celiac plexus:
- Hepatic plexus
- Splenic plexus
- Gastric plexus
- Pancreatic plexus
- Suprarenal plexus
The celiac plexus gives rise to other plexuses, including:
- Renal plexus
- Testicular plexus / ovarian plexus
- Superior mesenteric plexus
The celiac, superior mesenteric, and renal ganglia that surround the roots of the renal, superior mesenteric, and celiac trunk arteries make up the celiac plexus. These ganglia are also known as prevertebral (paraaortic) ganglia because of their paraaortic position. The larger celiac (solar) plexus is made up of the smaller celiac, superior mesenteric, and renal plexuses that are related to the ganglia.
Parasympathetic, sympathetic, and nociceptive fibers are out of origin by the celiac plexus. The vagus nerve (CN X) provides parasympathetic input to the celiac plexus, whereas the greater and lesser splanchnic nerves provide sympathetic input.
The abdominal aorta’s branches are surrounded by periarterial plexuses that allow the celiac plexus’s branches to reach their target organs. The inferior portion of the esophagus, stomach, pancreas, spleen, kidneys, liver, gallbladder, and small intestine is therefore supplied by the celiac plexus.
Function
The celiac plexus is responsible for transmitting visceral sensory impulses from the midgut and foregut, such as reflexes or discomfort. With its parasympathetic division, it stimulates peristalsis and digestion and increases gland secretion. The sympathetic division narrows blood arteries, prevents peristalsis, and reroutes blood to skeletal muscles.
Clinical Importance
Celiac plexus block
Because the celiac plexus nociceptive fibers are constantly stimulated, people with upper abdominal cancers or chronic pancreatitis frequently experience unbearable stomach discomfort. In these situations, a treatment technique that aids in reducing pain perception is celiac plexus block.
A small needle is inserted through the posterior abdominal wall to execute a celiac plexus block. After using an X-ray to guide them, the doctor injects the painkiller into the celiac plexus. Pain relief from this operation might last anywhere from a few weeks to several years.
FAQs
What is a celiac plexus?
A network of nerves behind the belly and in front of the spine is known as the celiac plexus. The pancreas, gallbladder, intestines, liver, and stomach are all connected to the neurological system by these nerves. Cancer growth may cause discomfort in these regions for patients.
Is the coeliac plexus sympathetic or parasympathetic?
Another sympathetic plexus that is often located just lateral to the aorta at the level of T12 and L1 is the celiac plexus. The celiac plexus is formed by a combination of the greater, lesser, and least splanchnic nerves with parasympathetic contributions from the vagus nerve.
Does the celiac plexus include the vagus nerve?
Additionally, we saw that both vagus nerves particularly connect to the celiac plexus in the RCG. From there, the vagal information passes via the prevertebral ganglia to the SON and the OPN to the ovaries.
What is the role of the celiac plexus?
The regulation of several visceral processes, including gastrointestinal functions, is mostly controlled by the celiac plexus. The stomach, liver, gallbladder, pancreas, spleen, and portions of the small and large intestines are among the abdominal organs that are elaborately innervated by the celiac plexus.
What is the coeliac plexus of the gallbladder?
The vagus nerve provides parasympathetic innervation, whereas the celiac plexus transports sympathetic and sensory fibers. Because the sphincter of Oddi relaxes in response to parasympathetic stimulation, the gallbladder contracts, and bile is secreted into the cystic duct.
What organ is responsible for celiac disease?
The small intestine is impacted by celiac disease. The majority of your food’s nutrients, including proteins like gluten, are absorbed here. However, gluten in the small intestine causes an immunological reaction in those with celiac disease.
References
Celiac plexus. (2023, November 3). Kenhub. https://www.kenhub.com/en/library/anatomy/celiac-plexus
Wikipedia contributors. (2024b, May 8). Celiac plexus. Wikipedia. https://en.wikipedia.org/wiki/Celiac_plexus